
The authors argue that the retroperitoneal lymphadenectomy increases the intraoperative and postoperative complications. There are no established data about lymphadenectomy during treatment of ECs and to what extent lymphadenectomy should be performed. The International Federation of Gynecology and Obstetrics (FIGO) staging of ECs revised in 2009 to include the pelvic and para-aortic lymphadenectomy (PPLND) as one of the most important prognostic factors in ECs. Lymph node evaluation is the key point in EC staging and prognosis.

Learn about lymph node status and breast cancer stage.Endometrial cancer (EC) is the most common gynecological cancer in Europe. The axillary lymph nodes are already known to contain cancer (for example, before surgery, a health care provider felt suspicious lymph nodes and a needle biopsy showed they contained cancer).A person can’t have a sentinel node biopsy (for example, an axillary dissection has been done in the past).In some cases, a sentinel node biopsy is not advised, and an axillary dissection is done instead.
Because it disrupts more of the normal tissue in the underarm area, axillary dissection is more likely to affect arm function and cause lymphedema.įor this reason, sentinel node biopsy is the preferred first step to check the axillary lymph nodes. Axillary dissection, sentinel node biopsy and risk of lymphedemaĪxillary dissection removes more axillary lymph nodes than a sentinel node biopsy does. IHC is only recommended for assessing lymph node status when the results of H&E staining are uncertain and sometimes, after neoadjuvant therapy. However, studies showed the small deposits of tumor cells identified by IHC were not useful in prognosis. In the past, a lab test called immunohistochemistry (IHC) was sometimes used to assess lymph node status. The most common way to assess pathologic lymph node status is a lab test called H&E staining. If you have a positive sentinel lymph node, talk with your health care team about whether you need an axillary dissection. Most people with one or more positive sentinel nodes who have a mastectomy will need an axillary dissection or radiation therapy to the axillary lymph nodes. (Whole breast radiation therapy treats part of the underarm area as well as the breast.) Some women with 1-2 positive sentinel nodes who have a lumpectomy and will have whole breast radiation therapy may not need axillary dissection.
The goals of axillary dissection are to check how many lymph nodes have cancer and to reduce the chances of cancer returning in the lymph nodes. More lymph nodes may be removed with a procedure called axillary dissection.
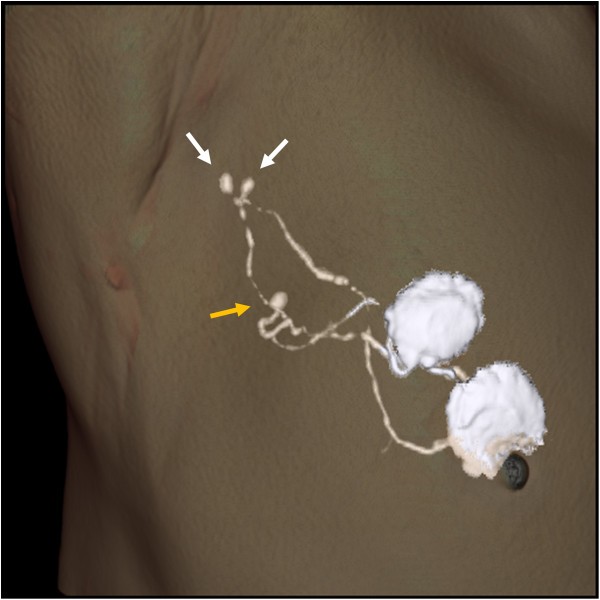
If the surgeon removes sentinel nodes, it doesn’t mean there’s cancer in the nodes. The surgeon removes the sentinel nodes and sends them to a pathologist. The radioactive tracer or blue dye usually identifies 1-5 nodes as the sentinel nodes. The surgeon locates the sentinel nodes by looking for the lymph nodes that have absorbed the tracer (using a special device called a gamma probe) or the dye (which turns the lymph nodes blue). These are also the first lymph nodes where breast cancer is likely to spread. The first axillary lymph nodes to absorb the tracer or dye are called the sentinel nodes. To check if cancer has spread to the axillary lymph nodes, most people have a procedure called sentinel node biopsy during breast surgery.īefore or during this procedure, a radioactive substance (called a tracer) and/or a blue dye is injected into the breast.


 0 kommentar(er)
0 kommentar(er)
